Whitening Treatment Options
Whitening options available to patients, including in-office whitening, take-home, and over-the-counter. The two key factors that influence whitening are concentration and exposure time. An increase in either of these two factors will increase the effects of the whitening gel to a certain degree.

Both in-office and take-home whitening are supervised by your dentist, starting with an initial consultation to determine initial shades of your teeth and followed by either in-office whitening, or dispensing take-home whitening with instructions.
In-office
During in-office whitening procedures, we treat the teeth with a high concentration hydrogen peroxide material (24-30%) while applying consistent heat in a controlled environment. The controlled environment isolates the whitening material to the teeth only, preventing leakage to the surrounding gums and tissues, thereby preventing sensitivity.
Temperature accelerates the reaction process leading shorter whitening treatment time (~30 minutes.) With shorter treatment times, there is less contact of the whitening material leading to less sensitivity. In-office whitening is able to achieve results in a very short period of time due to the highly concentrated materials and the utilization of heat.
Take-home
Take-home whitening utilizes custom fit trays which hold the whitening material against the tooth for extended periods of time (2 hours or more). The whitening material used to treat is a low concentration hydrogen peroxide (9%) or carbamide peroxide (10% – ⅓ of the strength of hydrogen peroxide) Take-home whitening takes advantage of exposure time, bathing the teeth in whitening gel for hours at a time. However, increased exposure time increases the likelihood sensitivity and for leakage to surrounding tissues.
However, take-home whitening is still effective with the disadvantages of sensitivity and increased treatment times.
Over the counter (OTC)
OTC treatments are available almost anywhere including the pharmacy, malls, and spas with no dental professional oversight. Extrinsic stains are not removed beforehand, concentrations are low, there is no customized whitening regimen, and the application of the material is not distributed equally among all teeth.
What is the biology behind natural tooth color?
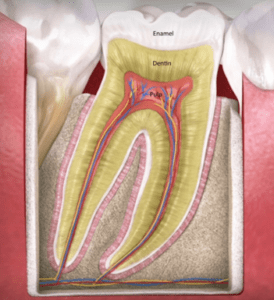
Your tooth has several layers that contribute to its color. Enamel is the characteristically white outer layer of your tooth that is visible to the eye. Dentin is the layer below the enamel which is naturally yellow in appearance. The inner chamber of the tooth is the pulp chamber which contains blood vessels, nutrients, and nerve fibers. The combination of these layers is what gives your tooth its natural color.
What causes discoloration of teeth?
A tooth’s color is a result of the convergence of anatomy and genetics of a tooth, environmental factors, and oral hygiene.
External stains are a result of stain molecules attaching to a bacterial biofilm on the tooth. This biofilm is the initial phase of plaque build-up and calculus build-up on your teeth. This biofilm is relatively easy to remove with good personal home care.
Some areas of the tooth may be inaccessible at home, and your dental hygienist will scrape away the plaque and calculus build-up which is the basis for these external stains. The teeth can discolor by the external stain penetrating the outer layer of the enamel. These discolorations are relatively easy to treat.
Internal stains aren’t a result of your diet and home hygiene, but are caused by genetics, aging, systemic conditions, environment, medications, and even trauma. These stains develop from the pulp layer and outward toward the dentin.
As you age, the pulp chamber shrinks and the dentin layer thickens, causing a more yellow appearance to the teeth due increased color from dentin. Medications can alter the color of teeth during development. Tetracycline is a drug used to treat bacterial infections, but when taken during tooth development, it can cause a gray or yellow stain deep within the tooth.
Trauma can cause damage within the pulp of the tooth, which can cause shrinkage of the pulp or even death of the nerve and vessels. The shrinkage of the pulp has the same effect of aging, where the colored dentin layer thickens. Death of the vessels and nerve chamber can cause darker staining of the dentin due to discolored remnants of the vessels and nerves.


What causes sensitivity when whitening?
There are several reasons that patients experience sensitivity after whitening such as:
- Contact of the surrounding gums and tissues with the whitening solutions
- Aggressive and improper use of heat causing reversible inflammation of the pulp
- Glycerine, ammonia, and acidic byproducts from the breakdown of carbamide peroxide (a common whitening solution)

Despite the various treatment options, the safest and most effective treatment is the “dual whitening” system which is dentist-prescribed and utilizes a combination of in-office whitening and take-home whitening. If you would like to learn more about teeth whitening, please contact us to schedule an appointment!